In ABA therapy, success isn’t just about quality care being delivered; it is about keeping the financial side clean and accurate. Many practices in therapy lose money not because of denied sessions but due to poor documentation and billing errors that could have been avoided.
Claims that are clear, detailed, and accurate move faster through the insurance process. And that’s what we call a clean claim-one that gets paid on the first submission without delays or denials.
But how does documentation actually affect those clean claim rates? Let’s break it down.
1. How Documentation Works in ABA Therapy Billing
In other words, documentation is the backbone of ABA therapy billing service. Every note, every timestamp, and every CPT code tells the payer what services were provided and why they’re medically necessary.
During the actual therapy session, behavior technicians or BCBAs chart session data, which details what goals are being addressed and minute spans. It might sound rather like routine; however, it certainly represents critical details that help the billing team or insurance reviewers move claims along.
Accurate data entry ensures clean claims, keeps RCM running well, and maintains compliance with the rules set by payers.At the same time, missing information, such as session duration or incorrect codes, leads to delays or even outright denials of payment.
That’s where companies like Pacemave make a difference by simplifying how providers manage their ABA billing service through structured documentation and automated checks.
2. What Happens When Documentation Fails
Inconsistent or incomplete documentation results in an impact on the billing process.
Here is what typically takes place:
- Claims get denied for mismatched data.
- Payments get delayed while insurance companies request for clarifications.
- Time is taken away from the therapists to revise their notes, which should instead go to the clients.
- Revenue cycles slow down, affecting cash flow and payroll schedules.
In other words, poor documentation leads to a domino-like effect wherein both care and business operations are compromised.
A reliable ABA therapy billing service prevents that by tracking every note, reviewing sessions before submission, and ensuring standards from insurance.
3. How proper documentation improves clean claim rates
When the documentation is done right, clean claim rates soar.
Here’s how it works in practice:
- Accurate session notes document what therapy was done and why.
- CPT codes and modifiers are applied correctly, reducing rejections.
- Real-time verification ensures a match of the data with the insurance requirements.
- Audit-ready records protect the provider from compliance issues.
This process doesn’t just help with faster reimbursements — it also builds trust between providers, payers, and families.
The steps listed above are integrated into a strong ABA therapy billing service, so your team doesn’t have to bother about clerical errors and repetitive paperwork.
If you want an even deeper level of insight into how these systems work behind the scenes, check out this Guide for ABA Therapy Provider
4. The Role of Credentialing and Denial Management
Proper documentation also supports two critical components of billing: credentialing and denial management.
Credentialing:
This is the process of registering your therapists with insurance payers. If credentialing data doesn’t match session records or claims, the system flags it as invalid-and payment stops right there.
Denial Management:
Organized documentation helps the billing team understand, even in cases of denial, what went wrong and allow for quick resubmissions. With clear records, denials become approvals faster.
Effective denial management combined with clean documentation will make your medical billing cycle strong, transparent, and predictable.
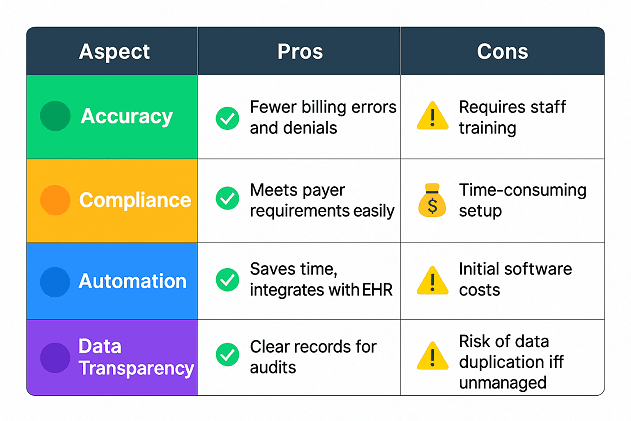
5. Pros and Cons of Documentation Systems
Let’s look at how documentation systems can impact billing efficiency.While some may find documentation demanding, the benefits far outweigh the challenges. Over time, accurate documentation leads to higher clean claim rates and smoother RCM workflows.
6. How We Handle Documentation the Smart Way
At Pacemave Efficiency and transparency are the drivers of our billing systems. We assist ABA providers in streamlining their ABA billing service by:
• Automating claim scrubbing and verification
• Tracking every documentation detail in real time
• Offering full denial management along with RCM support.
When the documentation flows cleanly, everything else follows: faster reimbursements, reduced administrative load, and better focus on client outcomes. If you’re interested in learning more about how billing ties to therapy coding and claim structure, please visit ABA Therapy Billing Service It’s a great source to understand the modern workflow of billing.
7. Final Thoughts
Documentation might not be the most exciting part of ABA therapy, but it’s the one that keeps your business stable and sustainable. Clean records mean clean claims, and clean claims mean a steady cash flow.
Accuracy is not optional in this evolving health care landscape; it is required. That is where a professional ABA therapy billing service bridges the gap between therapy sessions and successful reimbursements.
As the billing systems continue to modernize, today’s documentation will ensure fewer denials, stronger RCM, and smoother growth for providers in the future.